Novel Technology Breaks Up Problematic Calcium Within Plaque in the Leg Arteries
Lakeland Florida – 10/25/2022 – Surgical Center of Central Florida – in conjunction with Lakeland Vascular Institute, is now offering a novel treatment option for those suffering from an advanced form of peripheral artery disease (PAD) in which the plaque blockage also includes the presence of calcium. Intravascular Lithotripsy is an innovative advanced technology that uses sonic pressure waves to modify problematic calcium so that blockage can be alleviated and blood flow can be restored. The therapy leverages a similar minimally invasive approach that has been embraced by physicians for decades to treat kidney stones, which are also made up of calcium.
“We are thrilled to be among the first to offer this innovative technology, in an Ambulatory Surgery setting, to the patients of Lakeland and the surrounding communities of Polk County,” said Dr. Larry Whitney, “Hardened calcium within peripheral artery plaque is becoming more common as people are living longer and is very challenging to treat. The sonic pressure waves produced when performing Intravascular Lithotripsy gives us a novel, safe, and proven treatment option to break up the calcified plaque, with potentially less risk of injury to the vessel compared to other treatments.”
PAD affects nearly nine million people in the United States by preventing blood flow to the legs and feet, causing significant pain and limited mobility, and potentially leading to surgery or even amputation in severe cases. However, general awareness of PAD is estimated at only 25 percent based on prior studies. As the U.S. population continues to live longer, the incidence of calcium within these blockages is rising.
Calcium slowly develops and progresses to its hardened, bone-like state over the course of several decades of cellular growth and death in diseased plaque within the vessel walls. While it is slow to develop, its impact is immediately encountered when performing procedures to repair calcified plaques in the vessel. The calcium’s hardened structure restricts normal vessel movement and makes the rigid vascular tissue resistant to traditional balloon therapies that have been designed to compress the plaque within the vessel wall to restore normal blood flow. For these reasons, the presence of calcium increases the complexity of most cases and decreases the effectiveness of most treatments.
How Intravascular Lithotripsy (IVL) Works
Intravascular Lithotripsy uses a small generator to produce therapeutic sonic pressure waves from a catheter threaded through the vascular system to the site of the blockage. The pressure waves are inherently tissue-selective, passing through the soft vascular tissue, preferentially disrupting the hardened calcified plaque inside the vessel wall by creating a series of micro-fractures. After the calcium has been modified, the vessel can be expanded using a low-pressure balloon, thereby enabling even historically challenging PAD patients to be treated effectively with minimal injury to the vessel.
For an animation of the procedure, visit www.intravascularlithotripsy.com.
For more information, please visit our websites @ https://www.lvioutpatientcenter.com and https://surgicalcentercentralfl.com. Contact us today for a consultation at 863-577-0316.
CASE PERFORMED AT Surgical Center of Central Florida on 10/25/2022
P.B. is a 66-year-old former smoker who has a high-grade stenosis versus short segment occlusion of the right common iliac artery that was documented on a prior CT Angiogram as well as a prior aortogram performed at a local hospital. The patient had a previous attempt at the crossing of this suspected occlusion but was unsuccessful by outside practitioner. The patient was initially sent for evaluation for a femoral-to-femoral bypass by the CV surgeon, who referred to us for possible reattempt at revascularization. The patient presents with a severe lifestyle limiting intermittent claudication in the gluteal and proximal thigh region to 50 feet which are currently affecting her activities of daily living. She is also beginning to have a tingling sensation and some pain in her right foot, most pronounced at nighttime, bordering on ischemic rest pain. She presents today for revascularization of her right iliac artery, likely with intravascular lithotripsy and possible stenting, particularly given the heavy calcific coral reef type plaquing.
Angiogram: There is a 99% stenosis versus short segment occlusion of the right common iliac artery, which is heavily calcified, extending up to the level of the ostium.
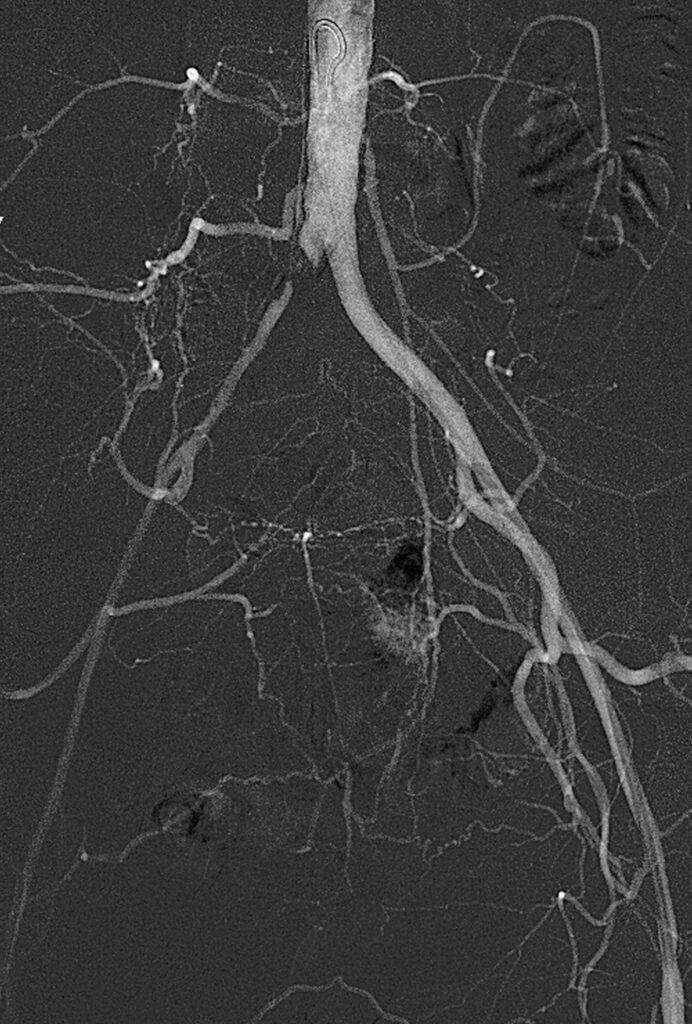
Treatment: Bilateral common femoral arterial access was obtained. A Seeker catheter and Glidewire combination were used to cross the occlusion from the right-side retrograde approach, and with some difficulty, I was able to eventually cross, and the catheter was advanced into the aorta where injection performed, revealing good intraluminal placement. We then upsized to a 6 French by 25 cm sheath, and heparin was given systemically. Over an 014 grand slam wire, we placed a 6 x 60 shockwave intravascular lithotripsy balloon. Given the fact that the plaque extended to the ostium and the concern for plaque shift with possible contralateral distal embolization, we elected to place a left-sided balloon for protection. Over an 035 wire, a 7 x 40 ultraverse balloon was placed up the left side. Balloon angioplasty was performed on the left side, followed by shockwave intravascular lithotripsy of the right common iliac artery. A total of 300 pulses were performed, and with 3-4 atm of pressure, we were able fully to expand the balloon with complete balloon width effacement. A follow-up arteriogram performed through an Omni flush catheter now reveals in-line flow through the right common iliac artery with a concurrent increase in size and perfusion. However, there continued to be marked irregularity and stenosis, at least in the range of 70% suspected with some recoil, and therefore we elected to deploy a stent to this area.

There was good stent expansion and good luminal caliber achieved, and a follow-up arteriogram revealed excellent in-line flow through the newly placed stent without evidence of significant encroachment on the contralateral side and no raising of the bifurcation. The patient had a palpable right femoral pulse immediately following stent deployment.

